Opioid-related statistics
reveal the U.S. has an enormous problem on its hands. Americans use 80 percent
of all the opioids sold worldwide.1 In
Alabama, which has the highest opioid prescription rate in the U.S., 143 prescriptions
are written for every 100 people.2 A
result of this over-prescription trend is skyrocketing deaths from overdoses.3,4
As recently reported by CNN,
the Manchester, New Hampshire, fire department responds to more calls for drug
overdoses than fires these days.5 In
2015, 52,404 Americans died from drug overdoses; 33,091 of them involved an
opioid and nearly one-third of them, 15,281, were by prescription.6,7,8
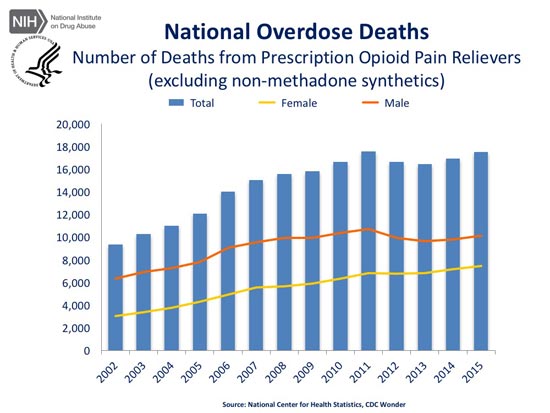
The following graph by the
National Institute on Drug Abuse shows the progressive incline in overdose
deaths related to opioid pain relievers between 2002 and 2015.9 This
does not include deaths from heroin addiction, which we now know is a common
side effect of getting hooked on these powerful prescription narcotics. In all,
we’re looking at just over 202,600 deaths in this 13-year time frame alone.10
Meanwhile, kidney disease,
listed as the ninth leading cause of death on the Center for Disease Control
and Prevention’s (CDC) top 10 list, killed
48,146.11 The
CDC does not include drug overdoses on this list, but if you did, drug
overdoses (63 percent of which are opioids), would replace kidney disease as the ninth leading cause
of death as of 2015. As if that wasn’t bad enough, recent statistics reveal
that in Americans under the age of 50, opioids are now the LEADING cause of death.
In a sadly ironic twist,
research reveals many other nations struggle with a dire lack of pain relief for
end-stage, terminal patients. As reported by The Atlantic:12 “Some
45 percent of the 56.2 million people who died in 2015 experienced serious
suffering, the authors found. That included 2.5 million children. More than 80
percent of the people were from developing regions, and the vast majority had
no access to palliative care and pain relief.”
Drug Enforcement Agency
Whistleblower Speaks Out
In a recent episode of 60
Minutes,13 whistleblower
Joe Rannazzisi lays the blame for the opioid crisis squarely on the shoulders
of the drug industry — especially the drug distributors — and Congress.14
It was well-known that drug
distributors were sending extraordinarily large shipments of opioids — hundreds
of millions of pills — to pharmacies across the U.S., and that people were
dying from their misuse; yet, rather than taking steps to stop the massacre,
industry lobbyists and Congress made it virtually impossible for agents at the
U.S. Drug Enforcement Agency (DEA) to take any action at all.
Rannazzisi should know. He
led the DEA’s Office of Diversion Control, which specifically regulates and
investigates the drug industry. According to Rannazzisi, “This is an industry
that’s out of control. What they want to do is do what they want to do, and not
worry about what the law is. And if they don’t follow the law in drug supply,
people die.” As reported by CBS News:15
“His greatest ire is reserved
for the distributors — some of them multibillion dollar, Fortune 500 companies.
They are the middlemen that ship the pain pills from manufacturers, like Purdue
Pharma and Johnson & Johnson to drug stores all over the country.
Rannazzisi accuses the distributors of fueling the opioid epidemic by turning a
blind eye to pain pills being diverted to illicit use.”
Drug Distributors Acted With
Full Knowledge
The three largest drug
distributors — Cardinal Health, McKesson and AmerisourceBergen — control as
much as 90 percent of the opioid distribution in the U.S., and according to
Rannazzisi, they were most certainly aware of the fact that the suspiciously
large orders they filled were killing tens of thousands of people each year.
The drug makers facilitated these killings as well, by falsely testifying to
their safety and low risk of addiction when used for pain.
This
lie allowed hundreds of thousands of Americans to become addicted and tens of
thousands die over the past two decades. As addiction rose, so did “pill mills”
— so-called pain clinics that did little more than distribute narcotics. In
Rannazzisi’s words, the rapid rise in opioid abuse “made the whole crack
epidemic look like nothing.” The main difference was that opioids were
distributed by medical professionals rather than street gangs.
Rannazzisi
was in charge of prosecuting doctors and pharmacists caught pandering the drugs
to addicts, yet as soon as one was taken off the street, another would take his
or her place. It did nothing to quench the epidemic. So, he decided to “move up
the food chain” and go after the distributors who, by law, are required to
report and stop suspicious orders. Unusually large or excessively frequent
orders both fit the bill of a suspicious order, and such orders were being
routinely filled without ever being reported to the DEA.
Jim
Geldhof, who worked at the DEA for 40 years, attests to the fact that
distributors shipped thousands of suspicious orders. One of the more obvious
examples include a pharmacy in Kermit, West Virginia, which ordered 9 million
hydrocodone pills over the course of two years. With a population of just 392
people, no one in their right mind could possibly mistake this for anything but
a drug distribution ring.
Between 2007 and 2012, more
than 12 million pills were also shipped to McDowell County in West Virginia, a
county with a population of 28,000 — enough for nearly 86 pills per capita per
year.16 According
to Geldhof, the DEA kept looking for “a good-faith effort” by drug distributors
“to do the right thing,” but there was none. “Greed always trumped compliance,”
he says. DEA efforts to improve compliance also came to naught. “They just flat
out ignored us,” Geldhof says.
Chump Change Fines Levied
In
2008, the DEA levied a $13.2 million fine against McKesson for the filling of
hundreds of suspicious orders totaling millions of pills. Cardinal Health was
also fined $34 million that same year. Such fines did nothing to stem the tide,
however. Earlier this year McKesson again agreed to pay a $150 million
settlement for the same violation — the largest fine ever levied against a drug
distributor.
The settlement also prevents
McKesson from selling controlled substances from distribution centers in
Colorado, Ohio, Michigan and Florida
“for multiple years,” and imposes “new and enhanced compliance obligations on
McKesson’s distribution system,” according to the U.S. Department of Justice.17 Still,
when you consider the enormous profits made by these companies — in 2008,
Cardinal Health was reporting $3.4 billion in annual revenue — even fines in
the tens of millions amount to chump change.
Drug Distributors Took Aim at
DEA
In all, distributors have
been slapped with fines in excess of $341 million over the past seven years,18 with
little effect. On the contrary, distributors started complaining to Congress
saying the DEA was “treating them like a foreign drug cartel.” In 2011,
Cardinal Health took aim at Rannazzisi personally. Four years later, after
having his authority greatly reduced, he resigned. As reported by CBS:
“The companies’ attorneys went
over his head and called his bosses at the Justice Department, who called in
Rannazzisi to have him explain his tactics. ‘And it infuriated me that I was
over there, trying to explain what my motives were or why I was going after
these corporations?
And when I went back to the
office, and I sat down with my staff, I basically said, ‘You know, I just got
questioned on why we’re doing … what we’re doing … [N]ow this is war. We’re
going after these people and we’re not going to stop’ …
Rannazzisi says the drug
industry used [industry] money and influence to pressure top lawyers at the DEA
to take a softer approach. Former DEA attorney Jonathan Novak said it
divided the litigation office. He said in 2013, he noticed a sea change in the
way prosecutions of big distributors were handled.
Cases his supervisors once
would have easily approved, now weren’t good enough … Novak prosecuted cases
brought to him by Joe Rannazzisi’s investigators. He said his caseload started
to slow down dramatically … [Jonathan Novak said:] ‘These were cases where the
evidence was crystal clear that there was wrongdoing going on.’ He said his
bosses started to bog down the system, demanding ever more evidence.”
Several Dozen DEA Officials
Have Taken Drug Industry Jobs
According to Novak, one of
the primary reasons for the slowdown in cases was the exodus of DEA lawyers
that took high-paying jobs working for the drug industry. At least 56 former
DEA and Department of Justice officials have been hired by the drug industry
since 2000.19 Once
on the industry’s side, they lobbied against the DEA, arguing the agency’s
cases were weak and didn’t stand a chance in court — even though they’d
consistently won most of their cases so far.
In
other words, these attorneys levied their insider knowledge of potential weak
points against their former employer to protect the industry — all while
prescription rates, addiction rates and opioid-related overdoses kept
increasing. But the industry wasn’t satisfied with slowing the DEA down to a
crawl. They wanted the agency off its back permanently. So, lobbyists started
working on Congress to enact legislation that would effectively eliminate the
DEA’s powers of enforcement.
DEA Stripped of Its Enforcement
Powers
Just such a law was passed in
April 2016. The Ensuring Patient Access and Effective Drug Enforcement Act
severely restricts the DEA’s ability to track and charge pharmacies and
wholesalers who are expanding the opioid epidemic.
As noted by Rannazzisi, if
you really wanted to harm the U.S. with drugs, “the only thing I could think of
that would immediately harm is to take the authority away from the
investigative agency that is trying to enforce the Controlled Substances Act
and the regulations implemented
under the act. And that’s what this bill did.”
As a
result of this legislation, the DEA no longer has the power to freeze
suspicious distribution of prescription narcotics. The law also effectively
prevents people at the top of the chain from being held accountable. Overall,
the DEA’s ability to go after wholesale distributors peddling narcotics to pill
mills is now nearly nonexistent. As noted by Novak, the Justice Department has
been rendered “toothless; I don’t know how they stop this now.”
The main sponsor of the law —
and a staunch advocate for the drug industry in general — was Rep. Tom Marino,
R-Pa., a former county and federal prosecutor nominated by President Trump to
become the next drug czar. Fortunately, this particular fox was not entrusted
with the hen house. In mid-October, Marino withdrew his name from
consideration.20
Marino No Longer in the Running
for Drug Czar
Marino’s decision came right
on the heels of this joint investigation by 60 Minutes and The Washington Post
— which identified Marino as a key player in getting the bill passed21 —
and President Trump’s announcement that his administration would look into the
allegations against Marino.22 As
noted by Charlie Brown, president of Consumers for Dental Choice and the World
Alliance for Mercury-Free Dentistry, in a private email to me:
“Now the real battle
begins. More important than the fate some Congressman from rural
Pennsylvania who works secretly against his own constituents is this bad law,
which Congress created hence only Congress can repeal. The handcuffs must
come off DEA’s power to act against heroin drug kingpins in the corporate
suites wearing their three-piece suits and lab coats — and the local
distributors whose names end in M.D. and DDS and MHA (Masters in Hospital
Administration).
A campaign to show
Congressional complicity in heroin must get to the grassroots; accountability
must begin. Congress is not tough on illegal drugs, passing laws that put
a pathetic drug user in prison for life; Congress is tough on drugs by cutting
off the supply and putting in prison the kingpins.”
Sen. Joe Manchin, D-W.Va.,
told The Washington Post23 he
was “horrified” by the revelations of the investigation, saying the true intent
of Marino’s bill was “camouflaged,” such that no one understood the effect it
would have on the opioid epidemic. “That bill has to be retracted, has to be
repealed,” Manchin said. Sen. Claire McCaskill, D-Mo., has announced she will
in fact introduce legislation to repeal it. Manchin has also suggested
Rannazzisi would be a good candidate to head the DEA.
It’s
worth noting the bill was actually written by former director of DEA litigation
and compliance practice, Linden Barber, one of the several dozen people who
swapped sides to work on behalf of the drug industry. His deep understanding of
the internal workings of the agency’s enforcement strategies is part of what
makes the law so effective in its ability to hinder DEA action against drug
companies and distributors.
President Renews Vow to Address
Opioid Epidemic
Drug
companies, distributors, drugstore chains and drug manufacturers also spent
$102 million lobbying for the bill, claiming the DEA was impeding patients’
ability to receive “needed medication.” With statistics clearly telling a
different story, it should have been easy to see through this ruse. Clearly, it
was (and is) far too easy to get your hands on these pills. Yet the drug
industry won, and when they win, they typically do so at the patients’ expense.
October 16, after the 60
Minutes interview aired, President Trump announced his intention to declare
opioid addiction a national emergency, thereby securing much-needed funds and
policy initiatives to address the burgeoning epidemic.24,25 He
had initially supported such a move back in August, and has defended
accusations of foot dragging by saying it involves a lot of time-consuming
work.
CVS Takes Affirmative Action
In related news, CVS Pharmacy
recently announced it will limit opioid prescriptions to a seven-day supply for
certain health conditions26—
nearly one-third of the average supply prescribed by U.S. doctors. As of 2015,
the average prescription for an opioid was 18 days’ worth.27 By
doing so, CVS becomes the first pharmacy chain to restrict doctors’ ability to
overprescribe the drugs. CVS pharmacists will also be required to:
- Discuss
the risks of addiction with patients
- Instruct
patients on secure storage and proper disposal
- Use
immediate-release formulations before dispensing extended-release
versions, to lower the patient’s risk of building tolerance
The
initiative is scheduled to roll out as of February 1, 2018. CVS is also
expanding its drug disposal collection program, adding an additional 750 kiosks
at pharmacies across the U.S., for a nationwide total of 1,500, and is pledging
an additional $2 million donation to medication-assisted treatment programs
offered by community health centers. Another previous noble action they did was
to refuse to sell cigarettes in their stores.
Despite Epidemic of
Opioid-Related Deaths, Doctors Are Still Being Paid to Increase Opioid Sales
Clearly,
to really rein in the problem of overprescriptions and addiction, doctors need
to change their prescription habits. Patients need to take greater
responsibility for their own well-being as well. More than 33,000 Americans were
killed by opioids in 2015, and nearly half of them involved a prescription for
the drugs.
Knowing that these drugs
carry the serious risk of addiction, abuse and overdose, they should be
prescribed sparingly and only for the most severe cases of pain, for which no
other options are available. Instead, they are often prescribed widely to treat
milder cases of chronic pain, such as that from osteoarthritis or back pain, the latter of which has turned into
a major “gateway condition” that traps unsuspecting patients in the grip of
addiction.
Unfortunately,
the current medical system heavily discourages doctors from making much-needed
changes in their prescription habits. Patient pain assessment plays a
significant role in a doctor’s quality of care indicator, and nothing will
eliminate pain as effectively as a narcotic. In other words, if patients report
not getting pain relief, a doctor’s rating will go down. On top of that, and in
the midst of this epidemic of opioid overdose deaths, drug companies are also
still paying physicians to boost opioid sales by writing more prescriptions.
According to a study
published in the American Journal of Public Health,28 between
August 2013 and December 2015, more than 375,000 nonresearch opioid-related
payments were made to more than 68,000 physicians, totaling in excess of $46
million. This amounts to 1 in 12 U.S. physicians collecting money from drug
companies producing prescription opioids.
The top 1 percent of
physicians received nearly 83 percent of the payments, and the drug fentanyl, a synthetic opioid that can be
anywhere from 500 to 1,000 percent more potent than morphine, was associated
with the highest payments. Many of the states struggling with the highest rates
of overdose deaths, such as Indiana, Ohio and New Jersey, were also those
showing the most opioid-related payments to physicians. This suggests there’s a
direct link between doctors’ kick-backs and patient addiction rates and deaths.
It’s also worth noting that a
significant amount of people get their first opioid prescription from their
dentist.29 This
is particularly true for teenagers and young adults.30 Half
of all opioids are also prescribed to people with mental health problems.31
Nondrug Solutions for Pain
Relief
It’s
extremely important to be fully aware of the addictive potential of opioid
drugs, and to seriously weigh your need for them. There are many other ways to
address pain. Below is a long list of suggestions. Clearly, there are times
when pain is so severe that a narcotic pain reliever may be warranted. But even
in those instances, the options that follow may allow you to at least reduce
the amount you take, or the frequency at which you need to take them.
If you are in pain that is tolerable,
please try these options first, before resorting to prescription painkillers of
any kind. If you need a pain reliever, consider an over-the-counter (OTC)
option. Research32 shows
prescription-strength naproxen (Naprosyn, sold OTC in lower dosages as Aleve)
provides the same pain relief as more dangerous narcotic painkillers. However,
while naproxen may be a better alternative to narcotic painkillers, it still
comes with a very long list of potential side effects,33 and
the risks increase with frequency of use.
Eliminate or radically reduce
most grains and sugars from your diet
Avoiding grains and sugars
will lower your insulin and leptin levels and decrease insulin and leptin
resistance, which is one of the most important reasons why inflammatory
prostaglandins are produced. That is why stopping sugar and sweets is so important
to controlling your pain and other types of chronic illnesses.
Take a high-quality,
animal-based omega-3 fat
Omega-3
fats are precursors to mediators of inflammation called prostaglandins. (In
fact, that is how anti-inflammatory painkillers work, by manipulating
prostaglandins.) Good sources include wild caught Alaskan salmon, sardines and
anchovies, which are all high in healthy omega-3s while being low in
contaminants such as mercury. As for supplements, my favorite is krill oil, as
it has a number of benefits superior to fish oil.
Optimize your sun exposure and
production of vitamin D
Optimize your vitamin D by
getting regular, appropriate sun exposure, which will work through a variety of
different mechanisms to reduce your pain. Sun exposure also has anti-inflammatory
and pain relieving effects that are unrelated to vitamin D production, and
these benefits cannot be obtained from a vitamin D supplement.
Red, near-, mid- and
far-infrared light therapy (photobiology) and/or infrared saunas may also be quite helpful
as it promotes and speeds tissue healing, even deep inside the body.
Medical cannabis
Medical marijuana has a long history as a
natural analgesic and is now legal in 29 states including Washington, D.C. You
can learn more about the laws in your state on medicalmarijuana.procon.org.34
Kratom
Kratom (Mitragyna speciosa)
is another plant remedy that has become a popular opioid substitute.35 In
August 2016, the U.S. Drug Enforcement Administration issued a notice saying it
was planning to ban kratom, listing it as a Schedule 1 controlled substance.
However, following massive outrage from kratom users who say opioids are their
only alternative, the agency reversed its decision.36
Kratom
is likely safer than an opioid for someone in serious and chronic pain.
However, it’s important to recognize that it is a psychoactive substance and
should not be used carelessly. There’s very little research showing how to use
it safely and effectively, and it may have a very different effect from one
person to the next.
Also,
while it may be useful for weaning people off opioids, kratom is in itself
addictive. So, while it appears to be a far safer alternative to opioids, it’s
still a powerful and potentially addictive substance. So please, do your own
research before trying it.
Emotional Freedom Techniques
(EFT)
EFT is
a drug-free approach for pain management of all kinds. EFT borrows from the
principles of acupuncture in that it helps you balance out your subtle energy
system. It helps resolve underlying, often subconscious, and negative emotions
that may be exacerbating your physical pain. By stimulating (tapping)
well-established acupuncture points with your fingertips, you rebalance your
energy system, which tends to dissipate pain.
Meditation and Mindfulness
Training
Among volunteers who had
never meditated before, those who attended four 20-minute classes to learn a
meditation technique called focused attention (a form of mindfulness meditation) experienced
significant pain relief — a 40 percent reduction in pain intensity and a 57
percent reduction in pain unpleasantness.37
Chiropractic
Many
studies have confirmed that chiropractic management is much safer and less
expensive than allopathic medical treatments, especially when used for pain
such as low back pain.
Qualified
chiropractic, osteopathic and naturopathic physicians are reliable, as they
have received extensive training in the management of musculoskeletal disorders
during their course of graduate health care training, which lasts between four
and six years. These health experts have comprehensive training in
musculoskeletal management.
Acupuncture
Research has discovered a
“clear and robust” effect of acupuncture in the treatment of back,
neck and shoulder pain, and osteoarthritis and headaches.
Physical therapy
Physical therapy has been shown
to be as good as surgery for painful conditions such as torn cartilage and
arthritis.
Foundation Training
Foundation training is an innovative
method developed by Dr. Eric Goodman to treat his own chronic low back pain.
It’s an excellent alternative to painkillers and surgery, as it actually
addresses the cause of the problem.
Massage
A systematic review and
meta-analysis published in the journal Pain Medicine included 60 high-quality
and seven low-quality studies that looked into the use of massage for various
types of pain, including muscle and bone pain, headaches, deep internal pain,
fibromyalgia pain and spinal cord pain.38
The
review revealed massage therapy relieves pain better than getting no treatment
at all. When compared to other pain treatments like acupuncture and physical
therapy, massage therapy still proved beneficial and had few side effects. In
addition to relieving pain, massage therapy also improved anxiety and
health-related quality of life.
Astaxanthin
Astaxanthin is one of the most effective fat-soluble antioxidants known.
It has very potent anti-inflammatory properties and in many cases works far
more effectively than anti-inflammatory drugs. Higher doses are typically
required and you may need 8 milligrams (mg) or more per day to achieve this
benefit.
Ginger
This
herb has potent anti-inflammatory activity and offers pain relief and
stomach-settling properties. Fresh ginger works well steeped in boiling water
as a tea or grated into vegetable juice.
Curcumin
In a study of osteoarthritis
patients, those who added 200 mg of curcumin a day to their treatment plan
had reduced pain and increased mobility. A past study also found that a
turmeric extract composed of curcuminoids blocked inflammatory pathways,
effectively preventing the overproduction of a protein that triggers swelling and
pain.39
Boswellia
Also
known as boswellin or “Indian frankincense,” this herb contains specific active
anti-inflammatory ingredients.
Bromelain
This
enzyme, found in pineapples, is a natural anti-inflammatory. It can be taken in
supplement form but eating fresh pineapple, including some of the
bromelain-rich stem, may also be helpful.
Cetyl Myristoleate (CMO)
This
oil, found in fish and dairy butter, acts as a joint lubricant and
anti-inflammatory. I have used this for myself to relieve ganglion cysts and
carpal tunnel syndrome. I used a topical preparation for this.
Evening Primrose, Black Currant
and Borage Oils
These
contain the essential fatty acid gamma-linolenic acid (GLA), which is
particularly useful for treating arthritic pain.
Cayenne Cream
Also
called capsaicin cream, this spice comes from dried hot peppers. It alleviates
pain by depleting the body’s supply of substance P, a chemical component of
nerve cells that transmits pain signals to your brain.
Methods such as hot and cold
packs, aquatic therapy, yoga, various mind-body techniques and cognitive
behavioral therapy40 can
also result in astonishing pain relief without drugs.
Grounding
Walking barefoot on the earth may also
provide a certain measure of pain relief by combating inflammation.
Mind-Body Therapies
Methods such as hot and cold
packs, aquatic therapy, yoga, various mind-body techniques and cognitive
behavioral therapy41 can
also result in astonishing pain relief without drugs.
Low-Dose Naltrexone (LDN)
Naltrexone
is an opiate antagonist, originally developed in the early 1960s for the
treatment of opioid addiction. When taken at very low doses (LDN, available
only by prescription), it triggers endorphin production, which can boost your
immune function and ease pain.